Do Osteoblasts Break Down or Build Bone Matrix? No Credit Lost Try Again
Affiliate nineteen. The Musculoskeletal Organization
19.2 Bone
Learning Objectives
Past the terminate of this department, you lot will exist able to:
- Allocate the different types of bones in the skeleton
- Explicate the role of the different jail cell types in bone
- Explain how bone forms during development
Bone, or osseous tissue, is a connective tissue that constitutes the endoskeleton. It contains specialized cells and a matrix of mineral salts and collagen fibers.
The mineral salts primarily include hydroxyapatite, a mineral formed from calcium phosphate. Calcification is the process of deposition of mineral salts on the collagen fiber matrix that crystallizes and hardens the tissue. The process of calcification only occurs in the presence of collagen fibers.
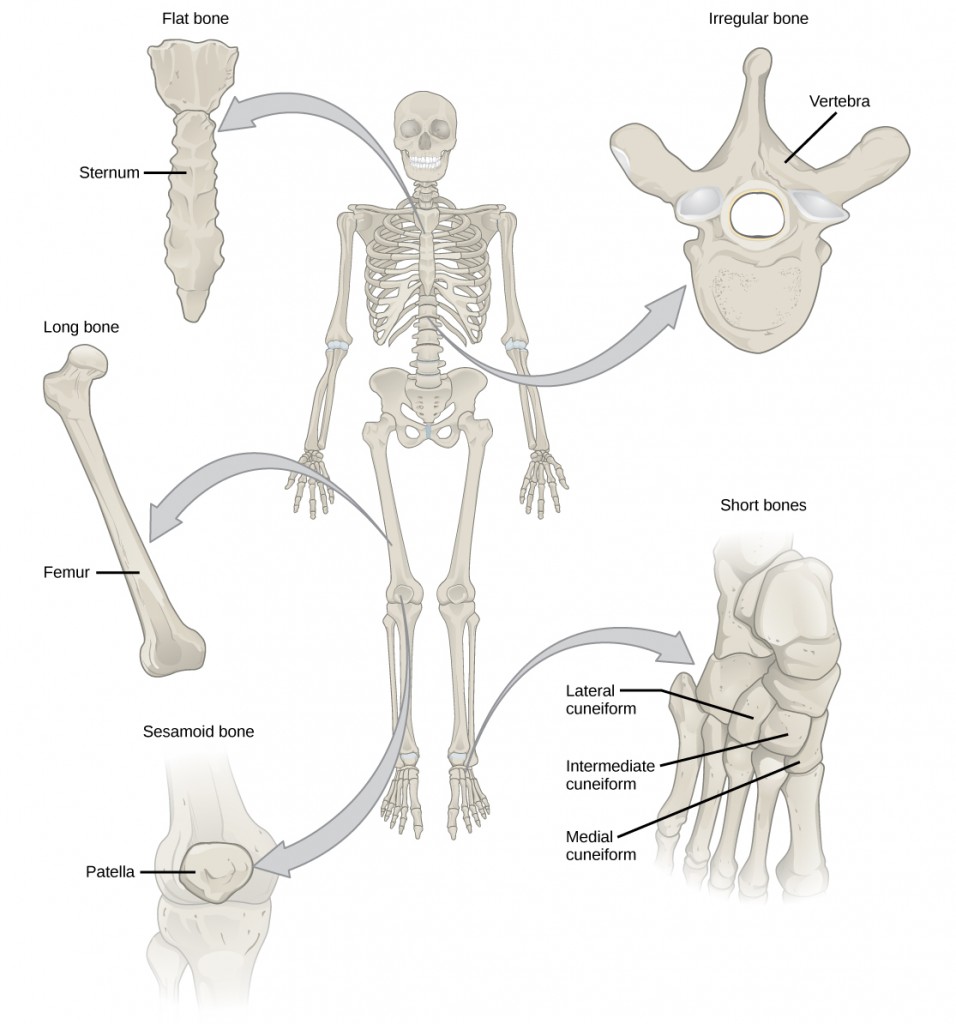
The bones of the man skeleton are classified by their shape: long bones, short bones, flat bones, sutural bones, sesamoid bones, and irregular basic (Figure 19.sixteen).
Long bones are longer than they are broad and have a shaft and ii ends. The diaphysis, or central shaft, contains bone marrow in a marrow cavity. The rounded ends, the epiphyses, are covered with articular cartilage and are filled with reddish os marrow, which produces blood cells (Figure 19.17). Virtually of the limb bones are long basic—for instance, the femur, tibia, ulna, and radius. Exceptions to this include the patella and the bones of the wrist and talocrural joint.
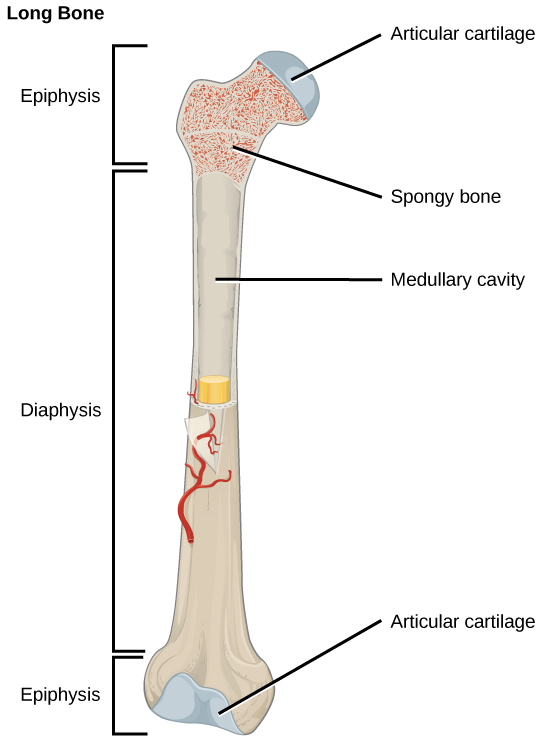
The long bone is covered past articular cartilage at either terminate and contains os marrow (shown in yellow in this illustration) in the marrow cavity.
Brusk bones, or cuboidal bones, are basic that are the same width and length, giving them a cube-like shape. For example, the bones of the wrist (carpals) and ankle (tarsals) are short bones (Figure 19.sixteen).
Flat bones are sparse and relatively broad basic that are found where extensive protection of organs is required or where broad surfaces of musculus attachment are required. Examples of flat bones are the sternum (chest os), ribs, scapulae (shoulder blades), and the roof of the skull (Figure 19.sixteen).
Irregular bones are bones with complex shapes. These bones may have short, flat, notched, or ridged surfaces. Examples of irregular bones are the vertebrae, hip basic, and several skull bones.
Sesamoid bones are small, flat basic and are shaped similarly to a sesame seed. The patellae are sesamoid bones (Effigy 19.18). Sesamoid basic develop inside tendons and may be found near joints at the knees, hands, and feet.

The patella of the genu is an example of a sesamoid bone.
Sutural bones are small, flat, irregularly shaped bones. They may be plant between the flat bones of the skull. They vary in number, shape, size, and position.
Bone Tissue
Bones are considered organs because they contain various types of tissue, such equally blood, connective tissue, nerves, and os tissue. Osteocytes, the living cells of bone tissue, form the mineral matrix of bones. There are two types of bone tissue: compact and spongy.
Compact Os Tissue
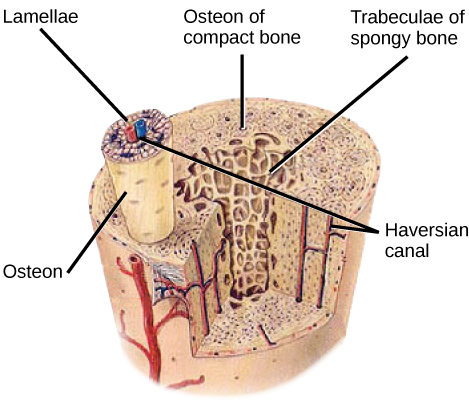
Compact bone (or cortical os) forms the hard external layer of all bones and surrounds the medullary crenel, or os marrow. Information technology provides protection and strength to bones. Compact bone tissue consists of units called osteons or Haversian systems. Osteons are cylindrical structures that comprise a mineral matrix and living osteocytes connected by canaliculi, which ship blood. They are aligned parallel to the long centrality of the bone. Each osteon consists of lamellae, which are layers of compact matrix that surround a central canal called the Haversian canal. The Haversian canal (osteonic canal) contains the bone's claret vessels and nerve fibers (Effigy xix.19). Osteons in compact bone tissue are aligned in the same direction along lines of stress and help the os resist bending or fracturing. Therefore, compact os tissue is prominent in areas of bone at which stresses are practical in only a few directions.
Which of the following statements about bone tissue is imitation?
- Meaty bone tissue is made of cylindrical osteons that are aligned such that they travel the length of the bone.
- Haversian canals incorporate blood vessels only.
- Haversian canals contain claret vessels and nervus fibers.
- Spongy tissue is plant on the interior of the os, and compact os tissue is found on the exterior.
Spongy Os Tissue
Whereas meaty bone tissue forms the outer layer of all bones, spongy os or cancellous bone forms the inner layer of all bones. Spongy bone tissue does not incorporate osteons that found compact bone tissue. Instead, information technology consists of trabeculae, which are lamellae that are arranged every bit rods or plates. Red bone marrow is found between the trabuculae. Blood vessels inside this tissue deliver nutrients to osteocytes and remove waste. The red bone marrow of the femur and the interior of other large bones, such as the ileum, forms blood cells.
Spongy os reduces the density of bone and allows the ends of long basic to shrink equally the result of stresses practical to the os. Spongy bone is prominent in areas of bones that are not heavily stressed or where stresses arrive from many directions. The epiphyses of basic, such equally the neck of the femur, are subject to stress from many directions. Imagine laying a heavy framed moving-picture show flat on the floor. You could hold up 1 side of the picture with a toothpick if the toothpick was perpendicular to the flooring and the picture. Now drill a hole and stick the toothpick into the wall to hang up the picture. In this instance, the part of the toothpick is to transmit the down pressure of the picture to the wall. The force on the picture is straight downwardly to the floor, but the force on the toothpick is both the picture wire pulling down and the lesser of the hole in the wall pushing up. The toothpick will interruption off correct at the wall.
The neck of the femur is horizontal like the toothpick in the wall. The weight of the body pushes information technology downwardly near the joint, but the vertical diaphysis of the femur pushes it upward at the other end. The cervix of the femur must be potent enough to transfer the downward forcefulness of the body weight horizontally to the vertical shaft of the femur (Figure 19.20).
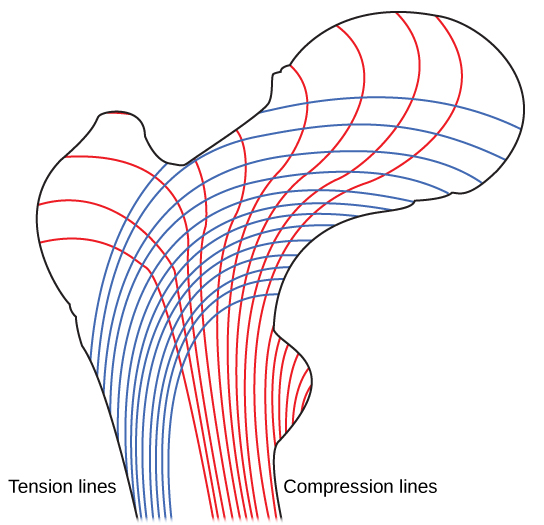
Trabeculae in spongy bone are arranged such that one side of the bone bears tension and the other withstands compression.
Concept in Action

View micrographs of musculoskeletal tissues as you review the beefcake.
Cell Types in Bones
Os consists of four types of cells: osteoblasts, osteoclasts, osteocytes, and osteoprogenitor cells. Osteoblasts are bone cells that are responsible for bone formation. Osteoblasts synthesize and secrete the organic function and inorganic function of the extracellular matrix of bone tissue, and collagen fibers. Osteoblasts get trapped in these secretions and differentiate into less agile osteocytes. Osteoclasts are large bone cells with upwardly to 50 nuclei. They remove os construction by releasing lysosomal enzymes and acids that dissolve the bony matrix. These minerals, released from basic into the blood, assistance regulate calcium concentrations in body fluids. Os may also exist resorbed for remodeling, if the applied stresses take changed. Osteocytes are mature bone cells and are the main cells in bony connective tissue; these cells cannot divide. Osteocytes maintain normal bone structure by recycling the mineral salts in the bony matrix. Osteoprogenitor cells are squamous stem cells that split to produce daughter cells that differentiate into osteoblasts. Osteoprogenitor cells are important in the repair of fractures.
Development of Os
Ossification, or osteogenesis, is the process of os formation by osteoblasts. Ossification is singled-out from the process of calcification; whereas calcification takes identify during the ossification of bones, information technology can also occur in other tissues. Ossification begins approximately six weeks afterward fertilization in an embryo. Earlier this fourth dimension, the embryonic skeleton consists entirely of fibrous membranes and hyaline cartilage. The development of bone from fibrous membranes is chosen intramembranous ossification; evolution from hyaline cartilage is called endochondral ossification. Os growth continues until approximately historic period 25. Bones can abound in thickness throughout life, but later historic period 25, ossification functions primarily in bone remodeling and repair.
Intramembranous Ossification
Intramembranous ossification is the process of bone evolution from fibrous membranes. Information technology is involved in the germination of the apartment bones of the skull, the mandible, and the clavicles. Ossification begins as mesenchymal cells form a template of the time to come os. They then differentiate into osteoblasts at the ossification eye. Osteoblasts secrete the extracellular matrix and deposit calcium, which hardens the matrix. The not-mineralized portion of the bone or osteoid continues to form around claret vessels, forming spongy os. Connective tissue in the matrix differentiates into reddish bone marrow in the fetus. The spongy bone is remodeled into a sparse layer of compact bone on the surface of the spongy bone.
Endochondral Ossification
Endochondral ossification
is the process of os development from hyaline cartilage. All of the bones of the torso, except for the flat bones of the skull, mandible, and clavicles, are formed through endochondral ossification.
In long basic, chondrocytes course a template of the hyaline cartilage diaphysis. Responding to complex developmental signals, the matrix begins to calcify. This calcification prevents diffusion of nutrients into the matrix, resulting in chondrocytes dying and the opening upwardly of cavities in the diaphysis cartilage. Blood vessels invade the cavities, and osteoblasts and osteoclasts change the calcified cartilage matrix into spongy bone. Osteoclasts and so suspension downwardly some of the spongy bone to create a marrow, or medullary, cavity in the middle of the diaphysis. Dense, irregular connective tissue forms a sheath (periosteum) around the bones. The periosteum assists in attaching the bone to surrounding tissues, tendons, and ligaments. The bone continues to abound and elongate every bit the cartilage cells at the epiphyses divide.
In the terminal stage of prenatal bone development, the centers of the epiphyses begin to calcify. Secondary ossification centers form in the epiphyses every bit blood vessels and osteoblasts enter these areas and catechumen hyaline cartilage into spongy bone. Until adolescence, hyaline cartilage persists at the epiphyseal plate (growth plate), which is the region between the diaphysis and epiphysis that is responsible for the lengthwise growth of long bones (Figure 19.21).
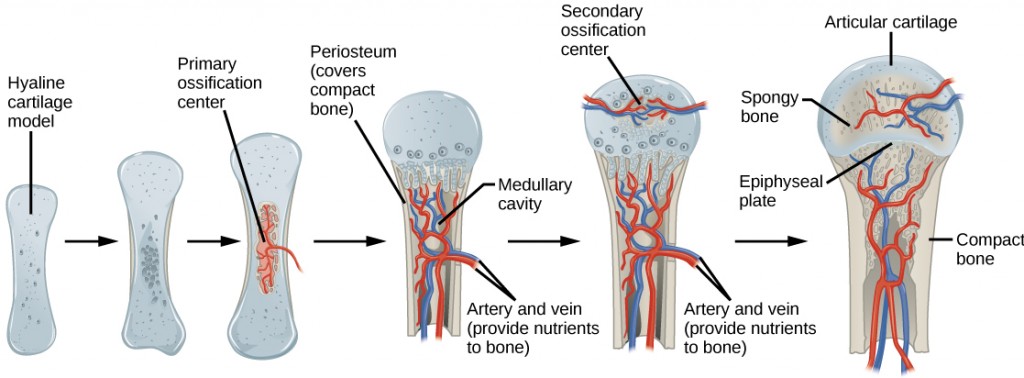
Endochondral ossification is the procedure of bone evolution from hyaline cartilage. The periosteum is the connective tissue on the outside of bone that acts as the interface betwixt bone, claret vessels, tendons, and ligaments.
Growth of Bone
Long basic go along to lengthen, potentially until adolescence, through the addition of bone tissue at the epiphyseal plate. They besides increment in width through appositional growth.
Lengthening of Long Basic
Chondrocytes on the epiphyseal side of the epiphyseal plate divide; one cell remains undifferentiated almost the epiphysis, and one jail cell moves toward the diaphysis. The cells, which are pushed from the epiphysis, mature and are destroyed by calcification. This process replaces cartilage with bone on the diaphyseal side of the plate, resulting in a lengthening of the bone.
Long bones stop growing at effectually the age of 18 in females and the age of 21 in males in a procedure called epiphyseal plate closure. During this process, cartilage cells stop dividing and all of the cartilage is replaced by bone. The epiphyseal plate fades, leaving a structure chosen the epiphyseal line or epiphyseal remnant, and the epiphysis and diaphysis fuse.
Thickening of Long Bones
Appositional growth is the increment in the diameter of bones by the add-on of bony tissue at the surface of bones. Osteoblasts at the bone surface secrete os matrix, and osteoclasts on the inner surface intermission down bone. The osteoblasts differentiate into osteocytes. A residue between these 2 processes allows the bone to thicken without becoming likewise heavy.
Os Remodeling and Repair
Bone renewal continues after nativity into adulthood. Bone remodeling is the replacement of old bone tissue past new bone tissue. Information technology involves the processes of bone deposition past osteoblasts and bone resorption past osteoclasts. Normal os growth requires vitamins D, C, and A, plus minerals such as calcium, phosphorous, and magnesium. Hormones such equally parathyroid hormone, growth hormone, and calcitonin are likewise required for proper os growth and maintenance.
Bone turnover rates are quite high, with five to vii percent of os mass being recycled every week. Differences in turnover rate be in different areas of the skeleton and in different areas of a bone. For example, the bone in the head of the femur may be fully replaced every six months, whereas the os along the shaft is altered much more slowly.
Bone remodeling allows bones to adapt to stresses by becoming thicker and stronger when subjected to stress. Bones that are non subject area to normal stress, for example when a limb is in a cast, will begin to lose mass. A fractured or cleaved bone undergoes repair through four stages:
- Claret vessels in the broken bone tear and hemorrhage, resulting in the germination of clotted blood, or a hematoma, at the site of the suspension. The severed blood vessels at the broken ends of the os are sealed by the clotting procedure, and bone cells that are deprived of nutrients begin to die.
- Within days of the fracture, capillaries grow into the hematoma, and phagocytic cells begin to clear away the dead cells. Though fragments of the claret jell may remain, fibroblasts and osteoblasts enter the expanse and begin to reform bone. Fibroblasts produce collagen fibers that connect the cleaved bone ends, and osteoblasts showtime to course spongy bone. The repair tissue between the cleaved bone ends is called the fibrocartilaginous callus, as it is equanimous of both hyaline and fibrocartilage (Effigy 19.22). Some bone spicules may also appear at this signal.
- The fibrocartilaginous callus is converted into a bony callus of spongy bone. It takes nearly two months for the broken bone ends to be firmly joined together after the fracture. This is similar to the endochondral germination of bone, equally cartilage becomes ossified; osteoblasts, osteoclasts, and bone matrix are present.
- The bony callus is then remodelled by osteoclasts and osteoblasts, with excess material on the outside of the os and within the medullary cavity beingness removed. Compact bone is added to create os tissue that is similar to the original, unbroken bone. This remodeling can take many months, and the bone may remain uneven for years.

Scientific Method Connection
Decalcification of Bones
Question: What effect does the removal of calcium and collagen have on os structure?
Background: Conduct a literature search on the role of calcium and collagen in maintaining bone construction. Acquit a literature search on diseases in which bone structure is compromised.
Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of basic that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium dorsum to decalcified bones.
Test the hypothesis: Test the prediction by removing calcium from chicken bones by placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified os by placing the decalcified chicken bones into a jar of water with calcium supplements added. Exam the prediction by denaturing the collagen from the basic by baking them at 250°C for three hours.
Analyze the information: Create a table showing the changes in bone flexibility, force, and mass in the three different environments.
Report the results: Under which conditions was the bone most flexible? Under which conditions was the bone the strongest?
Draw a determination: Did the results support or refute the hypothesis? How exercise the results observed in this experiment correspond to diseases that destroy bone tissue?
Summary
Bone, or osseous tissue, is connective tissue that includes specialized cells, mineral salts, and collagen fibers. The homo skeleton can be divided into long basic, brusk basic, flat bones, and irregular bones. Meaty bone tissue is composed of osteons and forms the external layer of all bones. Spongy os tissue is composed of trabeculae and forms the inner part of all bones. Iv types of cells compose bony tissue: osteocytes, osteoclasts, osteoprogenitor cells, and osteoblasts. Ossification is the process of os formation by osteoblasts. Intramembranous ossification is the process of bone development from fibrous membranes. Endochondral ossification is the procedure of os development from hyaline cartilage. Long bones lengthen every bit chondrocytes separate and secrete hyaline cartilage. Osteoblasts replace cartilage with bone. Appositional growth is the increase in the bore of bones by the addition of bone tissue at the surface of bones. Bone remodeling involves the processes of os deposition by osteoblasts and bone resorption by osteoclasts. Bone repair occurs in four stages and can take several months.
Exercises
- The Haversian canal:
- is arranged as rods or plates
- contains the bone'south blood vessels and nerve fibers
- is responsible for the lengthwise growth of long bones
- synthesizes and secretes matrix
- The epiphyseal plate:
- is arranged as rods or plates
- contains the bone's blood vessels and nervus fibers
- is responsible for the lengthwise growth of long bones
- synthesizes and secretes bone matrix
- The cells responsible for bone resorption are ________.
- osteoclasts
- osteoblasts
- fibroblasts
- osteocytes
- Meaty bone is composed of ________.
- trabeculae
- compacted collagen
- osteons
- calcium phosphate only
- What are the major differences betwixt spongy bone and compact os?
- What are the roles of osteoblasts, osteocytes, and osteoclasts?
Answers
- B
- C
- A
- C
- Compact bone tissue forms the hard external layer of all bones and consists of osteons. Compact bone tissue is prominent in areas of bone at which stresses are applied in only a few directions. Spongy bone tissue forms the inner layer of all bones and consists of trabeculae. Spongy bone is prominent in areas of bones that are non heavily stressed or at which stresses arrive from many directions.
- Osteocytes function in the substitution of nutrients and wastes with the blood. They too maintain normal bone structure by recycling the mineral salts in the bony matrix. Osteoclasts remove bone tissue by releasing lysosomal enzymes and acids that dissolve the bony matrix. Osteoblasts are bone cells that are responsible for os germination.
Glossary
- appositional growth
- increase in the diameter of bones past the improver of bone tissue at the surface of bones
- bone remodeling
- replacement of old bone tissue by new bone tissue
- os
- (also, osseous tissue) connective tissue that constitutes the endoskeleton
- calcification
- procedure of deposition of mineral salts in the collagen fiber matrix that crystallizes and hardens the tissue
- compact bone
- forms the difficult external layer of all bones
- diaphysis
- central shaft of bone, contains os marrow in a marrow cavity
- endochondral ossification
- process of bone development from hyaline cartilage
- epiphyseal plate
- region between the diaphysis and epiphysis that is responsible for the lengthwise growth of long bones
- epiphysis
- rounded end of bone, covered with articular cartilage and filled with red bone marrow, which produces claret cells
- flat bone
- sparse and relatively broad bone institute where extensive protection of organs is required or where broad surfaces of muscle attachment are required
- Haversian culvert
- contains the os's blood vessels and nervus fibers
- intramembranous ossification
- process of bone development from fibrous membranes
- irregular os
- os with complex shapes; examples include vertebrae and hip basic
- lamella
- layer of compact tissue that surrounds a fundamental culvert called the Haversian canal
- long bone
- bone that is longer than broad, and has a shaft and two ends
- osseous tissue
- connective tissue that constitutes the endoskeleton
- ossification
- (also, osteogenesis) process of bone formation by osteoblasts
- osteoblast
- bone cell responsible for bone formation
- osteoclast
- large bone cells with upward to 50 nuclei, responsible for bone remodeling
- osteocyte
- mature bone cells and the main prison cell in bone tissue
- osteon
- cylindrical structure aligned parallel to the long axis of the bone
- sesamoid bone
- small, apartment bone shaped like a sesame seed; develops inside tendons
- short bone
- os that has the same width and length, giving it a cube-similar shape
- spongy bone tissue
- forms the inner layer of all bones
- suture os
- pocket-sized, flat, irregularly shaped bone that forms between the flat bones of the attic
- trabeculae
- lamellae that are arranged every bit rods or plates
Source: https://opentextbc.ca/biology/chapter/19-2-bone/
0 Response to "Do Osteoblasts Break Down or Build Bone Matrix? No Credit Lost Try Again"
Post a Comment